The "Tingle" Gesture Recognition and Biofeedback Device is a project I'm working on at the Child Mind Institute. To put it very bluntly, it is designed to help kids stop compulsively tearing out their hair, a disorder called trichotillomania which is surprisingly prevalent. I built the prototype using the X9 activity tracker presented in this project.
From the MATTER Lab website:
As you are about to compulsively pull out your hair, bite your nails, or engage in some other body-focused repetitive behavior, you feel a tingle on your wrist. Then a notification is sent to an online dashboard. This information helps you to be mindful of your behavior as part of a behavior modification therapy, and helps your therapist monitor your progress. This is the rationale behind building the Tingle and applying for a patent. We have just run a pilot study and are preparing for a clinical trial.
Prevalence of body-focused repetitive behaviors (BFRBs)
Body-focused repetitive behaviors (BFRBs), symptoms of Obsessive Compulsive Disorder (OCD) and other conditions involving compulsions (e.g., Autism Spectrum Disorder) involve compulsively causing physical injury and/or damaging one’s physical appearance. These are among the most poorly understood symptoms; they are often misdiagnosed and undertreated. BFRBs include hitting oneself, biting, pulling out hair, skin picking and cutting, as well less severe but damaging behaviors such as nail biting, thumb sucking, and nose picking (Families & Health). These symptoms affect at least 5% of the population (Families & Health); hair pulling alone affects 1%, or about 3 million people in the US (Diefenbach, Reitman & Williamson 2002). BRFBs are highly comorbid. Studies have shown that as many as 70% of those with one BRFB will have another co-occurring BRFB (Conelea, Frank & Walther, 2017). While often impairing, affecting medical health and/or disfiguring, these symptoms are frequently reported but often not observed in clinical settings. This makes diagnosis, as well as treatment planning and monitoring, exceedingly difficult. To avoid pain and disfigurement, it is imperative to identify a reliable means to automatically identify and monitor BFRBs, especially outside the clinic setting. Clinicians need data on BFRB frequency and timing for the purposes of diagnosis, treatment planning and monitoring while patients need immediate, real-time feedback to make behavioral therapies more effective.
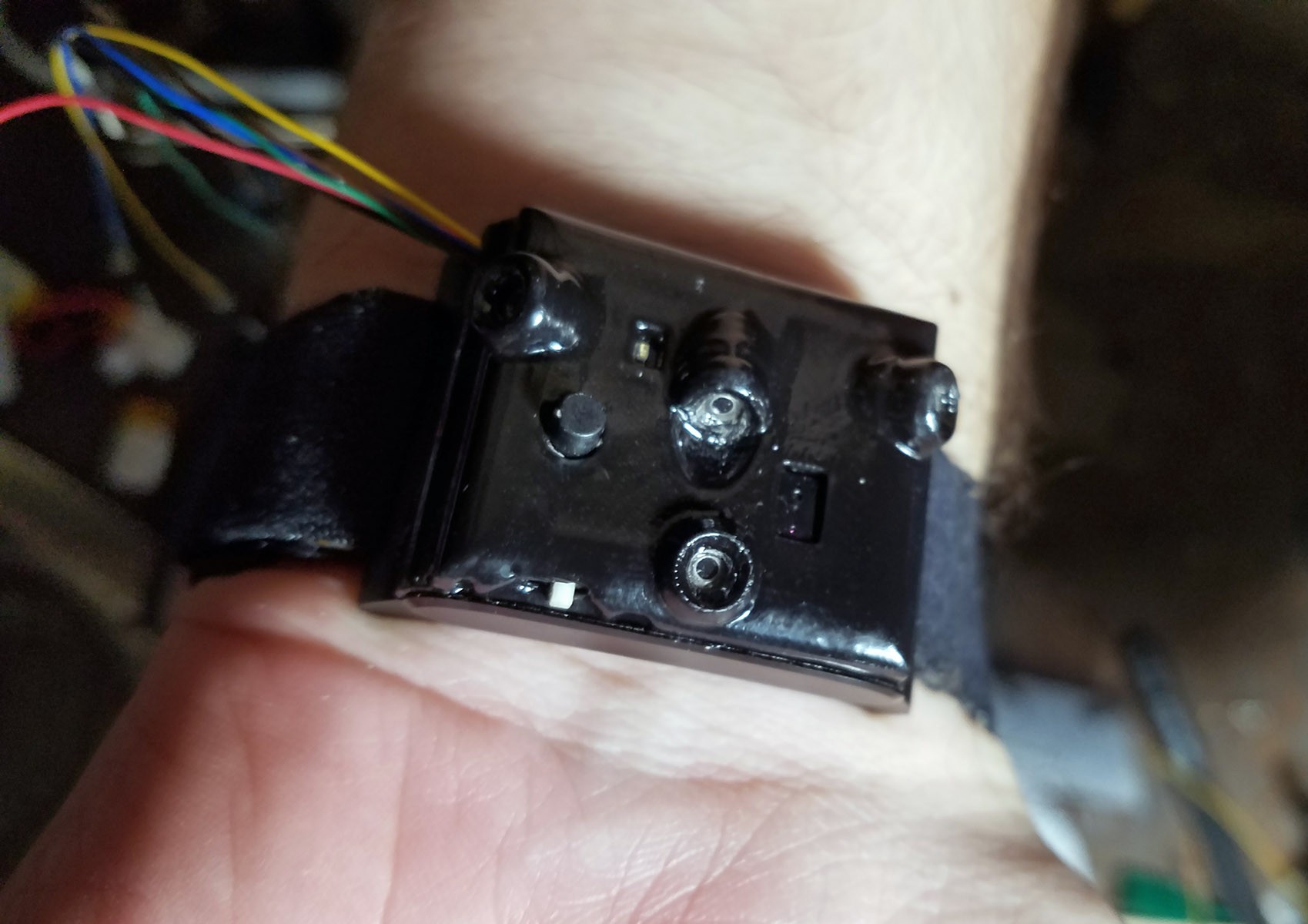
The “Tingle” device
To address this previously unmet clinical need, we have created a prototype for a wrist-worn device called the “Tingle” that can monitor and record BFRBs while also providing real-time (haptic) feedback (on the wrist) to the individual with BFRBs when they occur. The Tingle is the subject of U.S. Patent Application #15/816,706 filed January 26, 2018.
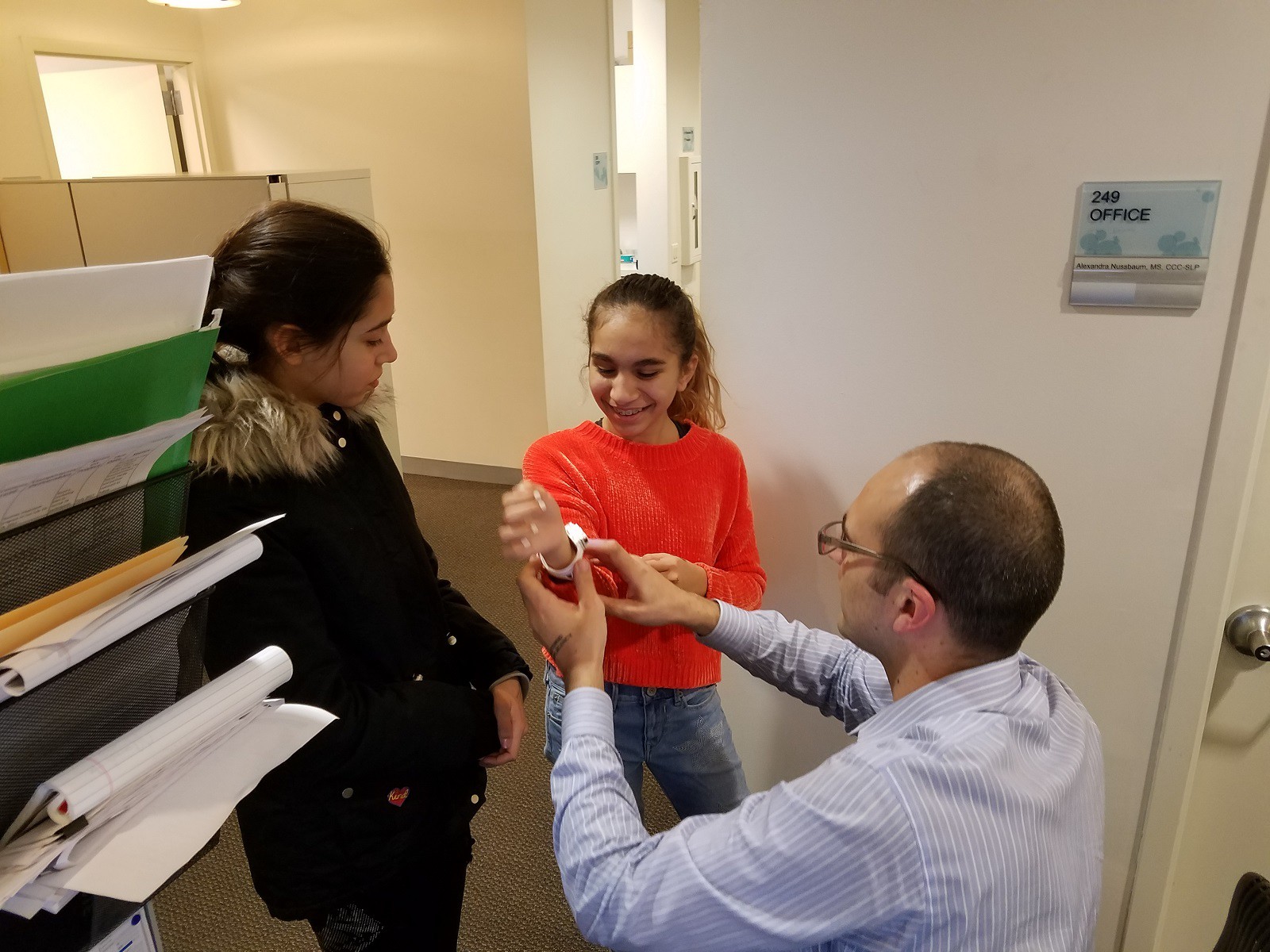
Testing the accuracy of the Tingle device for detecting different simulated BRFBs.
In a pilot study to establish the accuracy with which the Tingle can detect BFRBs in a controlled setting, we recruited 50 healthy, adult volunteers to wear the Tingle and repeatedly simulate 9 different behaviors (eating, smoking, thumb sucking, nail biting, nose picking, skin picking, and hair pulling from three locations). We just gathered the data and are analyzing the data now!
Testing the clinical efficacy of feedback via the Tingle in therapy.
This proof of concept leads to the critical next step of applying the Tingle to the clinical setting in which we will confirm the Tingle’s effectiveness in preparation for an FDA New Device Application and plan for commercialization. This will open the way for broad distribution in clinical practice as a diagnostic tool and to support the evaluation and implementation of pharmacological and behavior therapies for BFRBs.
Conclusion
The Tingle is well-positioned to address the tremendous unmet need in the care of individuals with BFRBs and other damaging and impairing compulsive behaviors. The Tingle will revolutionize the diagnosis and treatment of at least 5% of the population affected by these severe symptoms by using a convenient, automated, unobtrusive, and inexpensive device that both records behaviors for clinical assessment and provides accurate, real-time feedback to the wearer in support of therapy. We will evaluate the Tingle wearable device to facilitate diagnosis and therapy outside the clinic. In turn, this will facilitate the more rapid commercialization of this product to make it more widely available to clinicians and their patients.
References
- Conelea, Frank & Walther, 2017
- Diefenbach GJ1, Mouton-Odum S, Stanley MA. (2002). Affective correlates of trichotillomania. Behaviour Research and Therapy, 40(11). 2002 Nov;40(11):1305-15. doi:10.1016/S0005-7967(02)00006-2
- Families & Health Archived March 28, 2009, at the Wayback Machine., American Association for Marriage and Family Therapy [http://www.aamft.org:80/families/Consumer_Updates/Body-focusedRepetitiveDisorders.asp]

 Curt White
Curt White
Discussions
Become a Hackaday.io Member
Create an account to leave a comment. Already have an account? Log In.