In the wake of a disaster, there is a relative lack of rescuers and health providers and a surge of patients ranging from those with minor injuries to severe injuries. EMS systems use basic systems to classify (aka triage) patients according to the urgency treatment is needed and then move patients to areas where they can be treated accordingly. While awaiting transportation to a hospital, most patients are not monitored directly by a healthcare provider, but rather reassessed as often as possible by the providers available. In a catastrophic disaster like Hurricane Katrina, there were thousands of injured or ill/displaced people that required medical care, and an estimated 10,000 people were housed in the Houston Astrodome.
Imagine a scenario:
A massive earthquake leaves 2,000 people injured, nearly half with serious injuries. Regional hospital capacities are limited to 600 patients per day and the EMS system can transport approximately 40 patients per hour.
Twenty-five first responders arrive and the EMS system sets up a medical command center. Each first responder is given a backpack with 10 monitoring systems and an iPad along with basic first aid supplies. Each is assigned an area to operate. The first provider comes upon a patient with chest pain and a broken leg. They apply a triage tag to the patient and a monitoring device in 60 seconds. The iPad prompts them for a photo of the patient and a scan of the QR code located on the monitoring device. The patient is classified as yellow - needing urgent, but not immediate treatment. The provider moves on to the second victim, a child with serious bleeding from a fractured femur. The provider applies a pressure dressing to the bleeding and classifies the patient as red - needing immediate treatment. The provider moves on to the next victim.
At the central command station, patients begin to populate their monitoring screen. They see that a child has been labeled red and requires immediate treatment. They click on the patient and assign it to a treatment team. The treatment team consists of two providers and a backboard/cot, some advanced supplies, and an iPad. They receive notice via the iPad that they have been assigned to evacuate and care for the child and immediately receive directions to the zone where the patient is located. When in range, the iPad detects the WiFi or Bluetooth signal from the device and provides the team with a direction and distance to the patient. Once nearby, they ping the device to emit an loud noise so they can find the child quickly. They then evacuate the child to the main treatment and transportation area. The central monitoring station had already alerted a pediatric hospital and transport team which are awaiting the child when they arrive at the treatment area. A wifi network is quickly setup that covers the disaster area with numerous towers allowing triangulation of patient location with accuracy within 5 square feet.
After about two hours, the hospital and EMS systems are at capacity and cannot accept more patients. The treatment area will have to suffice as the hospital for now. A team of 15 providers are now tasked with caring for 400 patients with mild to moderate injuries. Instead of walking patient to patient, they each monitor a feed of the heart rate, respiratory rate, and oxygen saturation of a group of patients via laptop or tablet. If there is a worsening trend in their vitals, they go to the patient and assess and treat if needed. If patients are worsening rapidly, they identify them as priority for transportation when available. As they are able, they add medical information to the patients "chart" that can be used to monitor for problems - for example, if the first patient with chest pain has a history of seizures, medications can be allocated to the team to ensure the patient does not have seizures due to not having their medications.
The child is later identified by another victim of the quake as their child. The records are linked...
Read more » thomas.fogarty
thomas.fogarty


 Enrico Miglino
Enrico Miglino
 Brad Spry
Brad Spry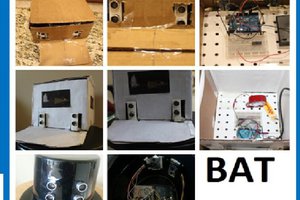
Looks like great product, especially that BOM!!